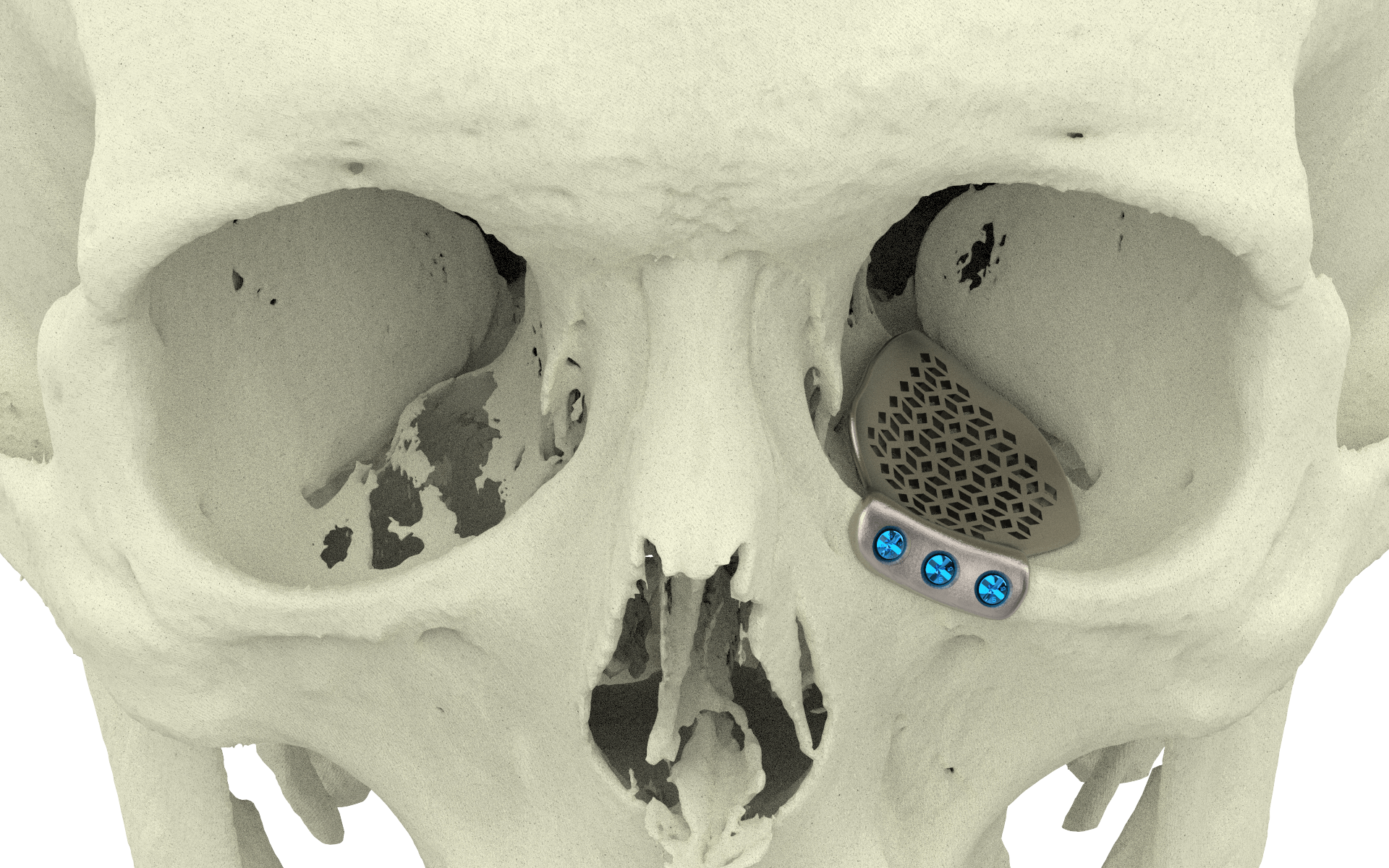
One Piece Orbital Floor
Orbital wall fractures can result in increased orbital volume, tissue herniation into the maxillary sinus, fat atrophy, loss of ligament support, and scar contracture leading to enophthalmos and diplopia. Reconstruction of large defects remains challenging since anatomical landmarks are lost, particularly the posteromedial orbital bulge and orbital apex.



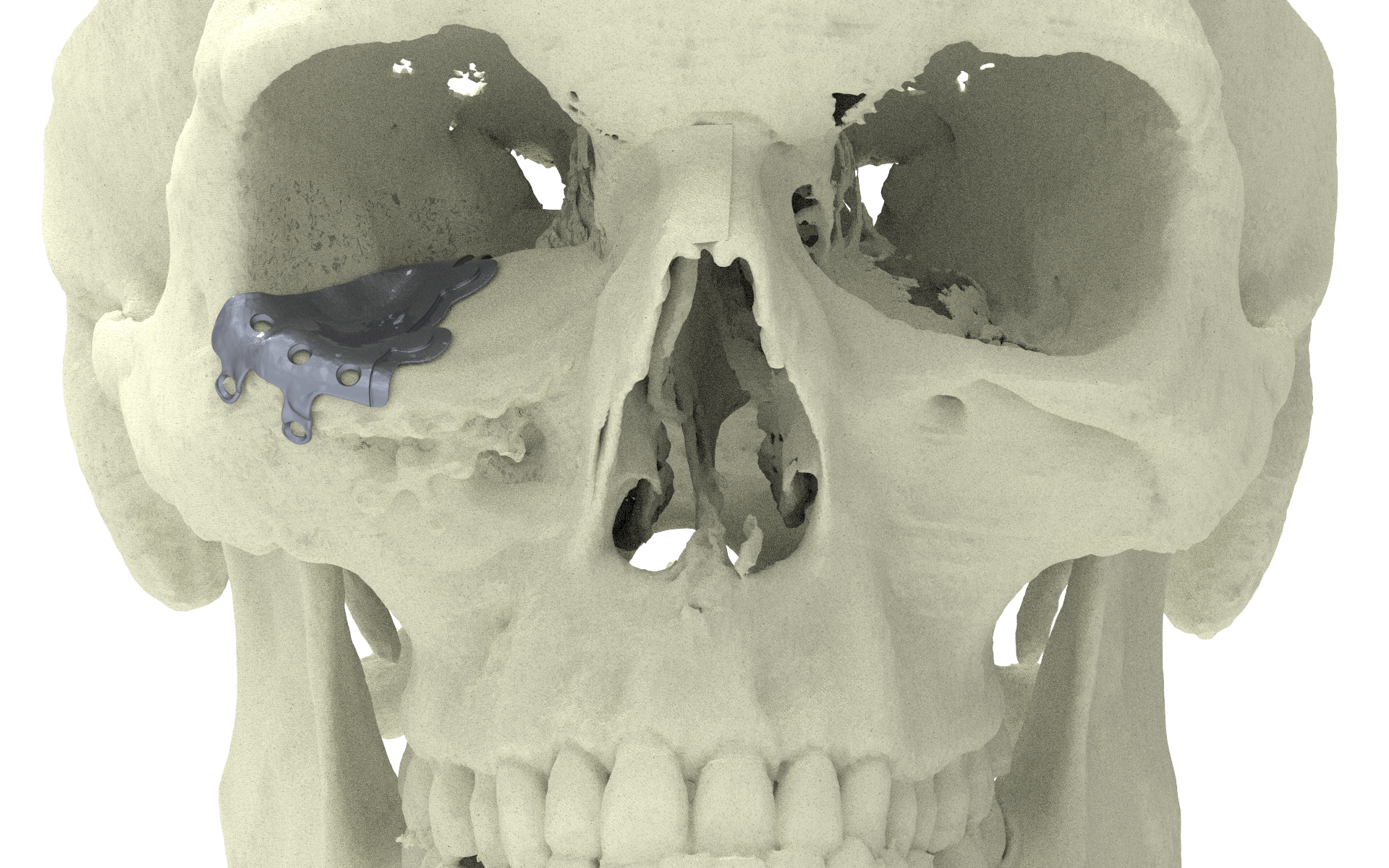
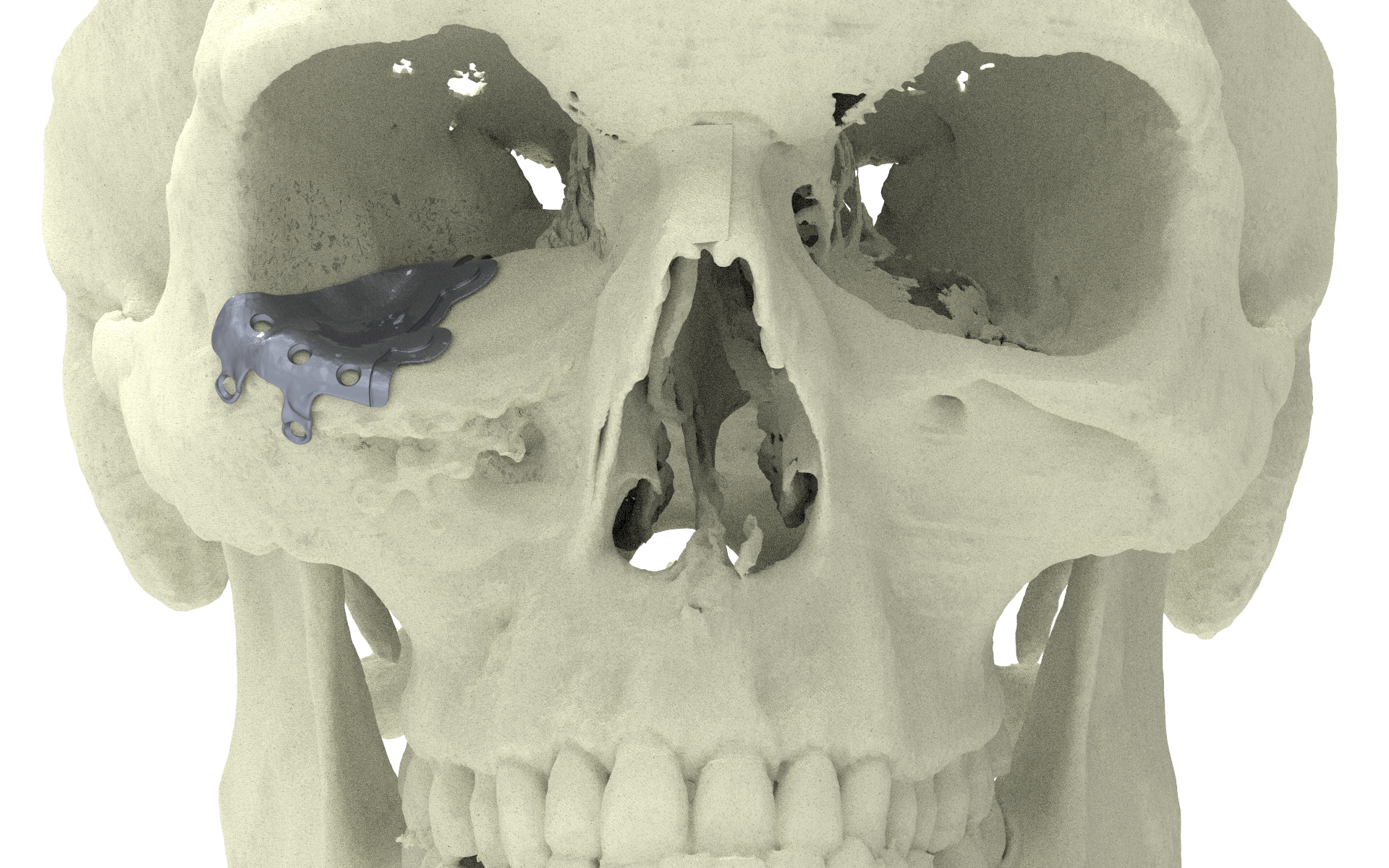
Two Piece Orbital Floor
Unfortunately nowadays standard pre bend meshes are used and often leave unsatisfied results.
PSI placement over failed pre bend mesh
To design implants for orbital reconstruction, rapid prototype models can be derived from Digital Imaging and Communications in Medicine (DICOM) data obtained from the patient’s computed tomography (CT) scan. The model is used to create the implant by mirroring data from the unaffected orbit, and reconstruction is performed with prebent plates. Although this technique is not commonly used, advantages include a true-to-original anatomical repair, restoration of orbital volume, and superior ophthalmological rehabilitation when evaluating for binocular single vision and ocular motility. From a surgical point of view, insertion is simplified by the precise fit, and no operating time is wasted in shaping the implant.




Mirror Orbital Floor
Left orbit was used to reconstruct the orbital floor on the defect side.
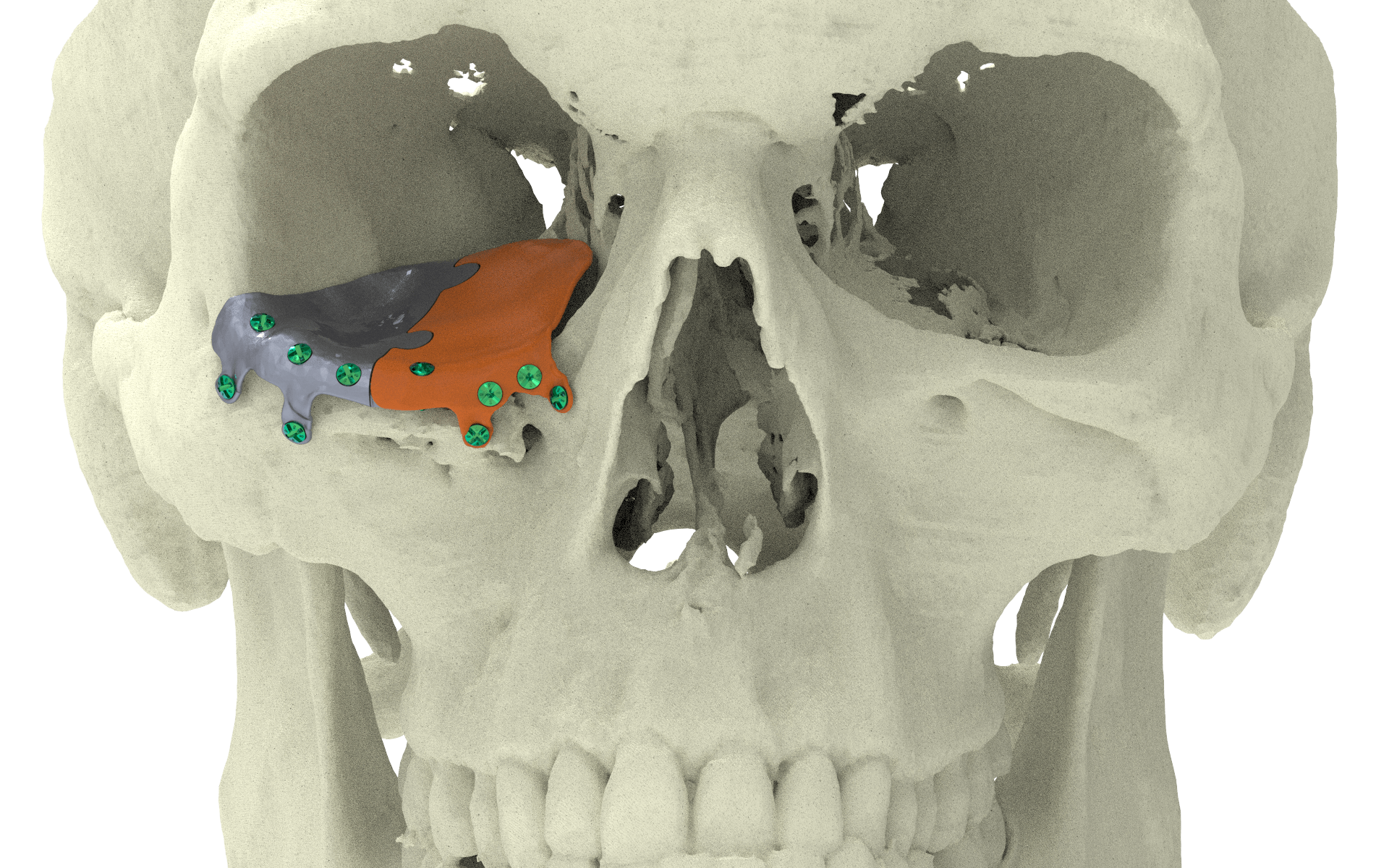
Lateral patient specific implant
Lateral implant placement.


Medial patient specific implant
The puzzle-like interlocking of the implant pieces allows unambiguous anteroposterior positioning of one piece relative to the other. Overlapping edges of the connection provide an interlock in the coronal plane, avoiding downward rotation of the connection when manually adapted
Fixation of the patient specific implant
Fixation screws were used to fixate the implant parts.
The puzzle design allows for accurate interlocking and good fit; implant overlap with the surrounding bone and overlap between pieces ensure a proper fit without the need for intraoperative navigation; a fixation screw inside the orbital rim stabilizes the first implant while the second piece is fitted; two screw holes per piece are optimal.



Happy patient
A patient who received this implant treatment regained his eyesight.
A 28-year-old man was referred with disabling diplopia and severe globe malposition after two repairs of an impure orbital floor fracture using a stock titanium orbital mesh plate. He had been hit by a pulley in a work accident. The presence of the previously inserted titanium mesh slightly hindered implant design because of the scatter effect on CT scan. Mirroring revealed a height difference of 7 mm between the unaffected side and the mesh on the affected side. The 3D model had to take into account the lower position of the orbital rim, and the screw position was based on the amount of remaining bone and positions of the mesh, infraorbital canal, and lacrimal system. The porous implants were printed with a double tongue-in-groove design. The puzzle-piece design allowed precise fit between the first and second implants. Anterior flanges were not necessary as the shape of the reconstructed infraorbital rim provided anteroposterior guidance.














